10 A mazing ways VR for pain relief is transforming health care
The Surprising New Way We’re Managing Pain
Just ten years ago, virtual reality was mostly about gaming, putting on a headset, waving controllers, and having fun with friends at a café. However, in 2025, VR has become a powerful tool in healthcare, enabling patients to manage pain during surgery, chemotherapy, and even childbirth.
I watched a young mother in the delivery room using virtual reality to help manage her labor discomfort. Instead of staring at a hospital ceiling, she was transported to a sunny beach, feeling warm sand under her toes and hearing seagulls overhead.
This isn’t a gimmick or a passing trend. For many patients, VR therapy transforms unbearable pain into manageable comfort, allowing them to breathe through discomfort instead of clenching their teeth.
What Exactly is VR Therapy?
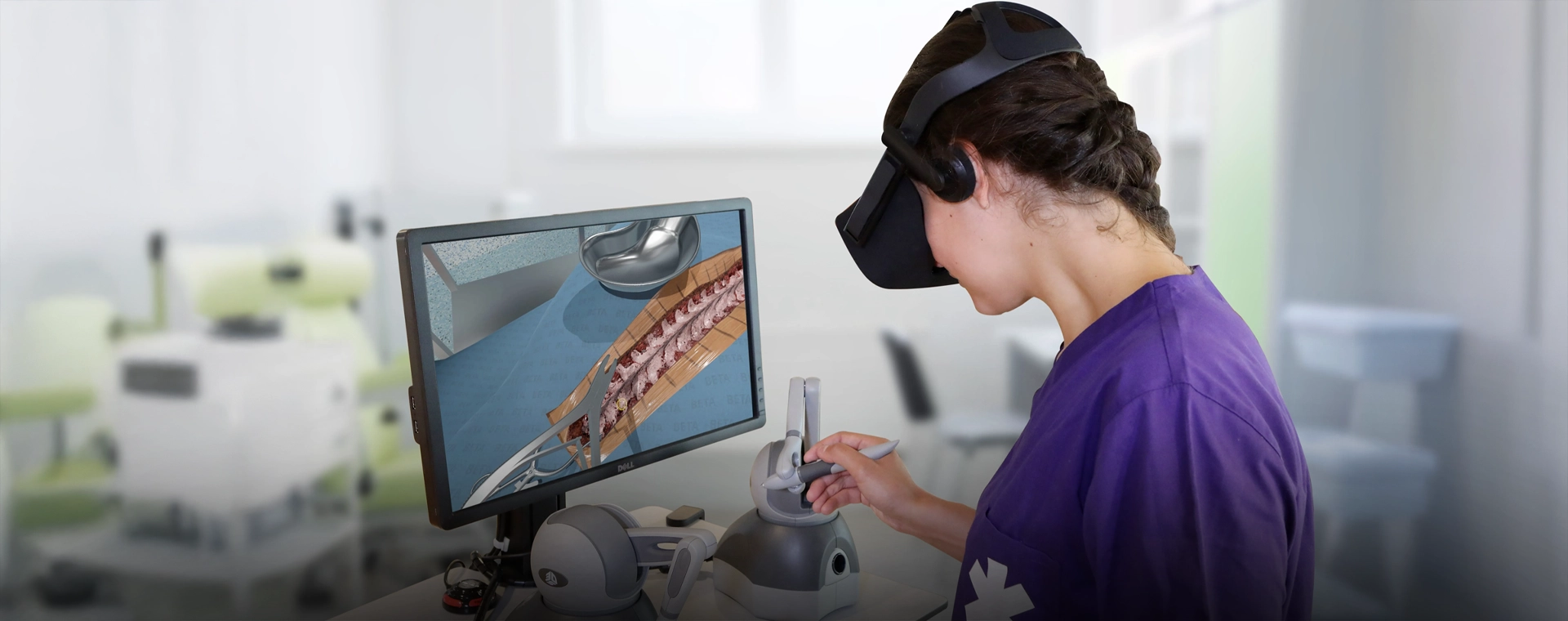
VR therapy combines a headset, motion sensors, and immersive software to transport patients to calming virtual environments, whether that’s a tranquil redwood forest after rain, the colorful shimmer of an underwater reef, or the vast quiet of outer space.
It’s like giving your mind a mental passport to escape pain, even while your body stays in bed healing.
From Bulky Gadgets to Bedside Care: A Short History
In the 1990s, VR in medicine was more experimental than practical clunky headsets, low-quality graphics, and sky-high costs that limited widespread use.
By 2025, VR headsets have become small enough to slip into a nurse’s kit, offering lifelike visuals that fully draw patients into the experience. Many hospitals now consider VR an essential medical tool, often found right alongside blood pressure monitors in patient rooms.
Why VR Works for Pain: The Science
Your Brain Can’t Fully Focus on Pain and Wonder at the Same Time
Pain is processed not only in your nerves but also in your brain. When VR floods your senses with engaging sights and sounds, your brain’s attention is fully occupied, leaving less “space” for pain signals.
The Ultimate Distraction
Think about getting so absorbed in a movie that you forget you’re hungry.VR takes that concept and elevates it to an entirely new dimension.
One burn patient shared, “When I was in the snow world, I forgot about the nurse changing my bandages. I could almost feel the cold.”
Proof It’s Not Just Hype
At Seattle Children’s Hospital, burn patients reported significantly less pain during dressing changes when using VR.
At Cedars-Sinai Medical Center, post-surgery patients experienced a 24% reduction in pain after VR therapy sessions.
Real people, real relief.
Top 5 Ways VR is Used for Pain Relief in 2025
1. Chronic Pain Management
From arthritis to fibromyalgia and back pain, VR helps patients manage symptoms without relying solely on medication. A 52-year-old woman with fibromyalgia told me, “It’s the only way I can get through my stretching without giving up.”
2. Post-Surgery Recovery
Rehabilitation after surgery often means painful movement. VR turns those exercises into engaging quests, making rehab less daunting.
3. Labor & Childbirth
Expectant mothers use VR-guided breathing and soothing visuals; some describe it as “a hand that never gets tired.”
4. Burn Injury Treatment
Dressing changes are intensely painful. VR lets patients “step outside” their pain. One boy recovering from a kitchen accident said, “I was in a jungle. I could hear monkeys. I didn’t want to come back.”
5. Cancer Treatment Support
Chemotherapy and radiation can be exhausting. VR offers distraction, meditation, and even social games to help pass the time and reduce stress.
Why Patients Love VR Therapy
No needles. No bitter-tasting medicine.
Reduced reliance on opioids - a major win for public health.
It feels engaging and playful - not clinical or intimidating.
But It’s Not Perfect… Yet
Cost: High-end clinical VR devices remain expensive.
Tech Comfort: Some patients, especially older adults, may need time to get used to the technology.
Research: More extensive studies are required to gain a complete understanding of VR’s long-term effects.
The Future Is Even More Exciting
AI-Powered VR: Software that adapts in real time to your pain level and mood.
Home VR Kits: Enabling daily self-managed pain relief sessions.
Telehealth Integration: Doctors can remotely prescribe VR therapy sessions, broadening access.
Voices from the Frontline
Dr. Lisa Morgan, a pain specialist, says:
“For patients who can’t tolerate strong medications, VR therapy can be a lifesaver.”
A cancer patient called it “a mental escape button.” A burn patient shared, “When I saw snow falling, I forgot I was in the hospital.”
Quick FAQs
Is VR therapy safe?
Yes, for most people those with epilepsy or pronounced motion sickness should seek medical advice before trying it.
How long is a session?
Usually between 10 and 30 minutes.
Can VR replace medication entirely?
Not yet, but it can significantly reduce the amount needed.
Is VR therapy covered by insurance?
Some providers cover it; coverage is growing.
Future of VR in Pain Management

We’re just scratching the surface. Currently, VR mainly supports distraction therapy, meditation, and patient education. Soon, it could help stroke patients relearn motor skills or let chronic pain sufferers visit personalized “comfort worlds” anytime from home.
With portable headsets becoming more affordable, VR for pain relief might become as commonplace as using a meditation app
Imagine turning pain into peace in under a minute, all from your chair.
Pain can stretch out moments like hours. VR bends time back to give relief
Whether it’s a burn patient transported to a snowy forest, a mother in labor breathing with ocean waves, or a chemo patient wandering a sunlit meadow, these aren’t just visuals; they’re moments of dignity and calm.
VR is no longer just “technology.”
